Physiotherapy for Bladder Control
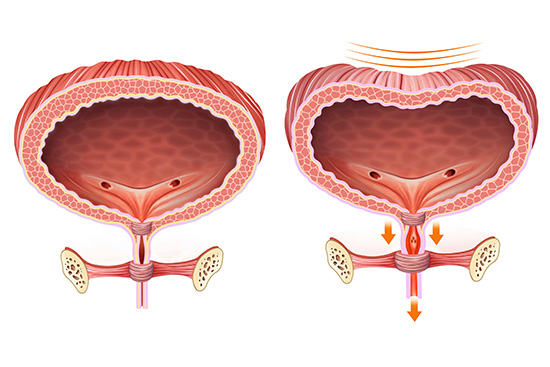
The Bladder
The bladder is a balloon shaped muscle, which stores urine. First sensation to empty the bladder should be at approximately 200mls. It should be possible to hold the urine comfortably to 350mls without having a strong urge to pass urine. The capacity of the bladder should be around 500mls. You should be able to walk to the toilet simply with a feeling of fullness and not feel like you have to run to get there with fear that you might leak.
As the bladder fills to capacity, it gives a sensation to pass urine. By tightening your pelvic floor muscles you should be able to delay the urge and postpone emptying the bladder until it is convenient. It is normal to empty your bladder 5-7 times in the day and once at night. There are a few different types of problems that can happen with the pelvic floor:
- Stress incontinence - this is loss of urine related to physical exertion
e.g. cough and sneeze or activities of daily living or exercise.
Download information on stress urinary incontinence - Urgency - this is an increased sense of urge in the bladder often at low
volumes of filling and related to triggers such as seeing the hall door or the toilet
door.
Download information on overactive bladder - Urge incontinence - this is the urgency at low volumes of filling as above but this time not quite making it to the toilet in time.
- Frequency - this is going to the toilet too often i.e. more than the maximum of eight times in a 24 hour period.
PDF Infographic Download
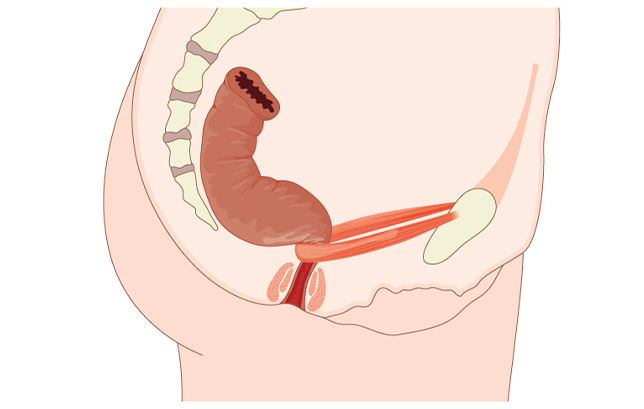
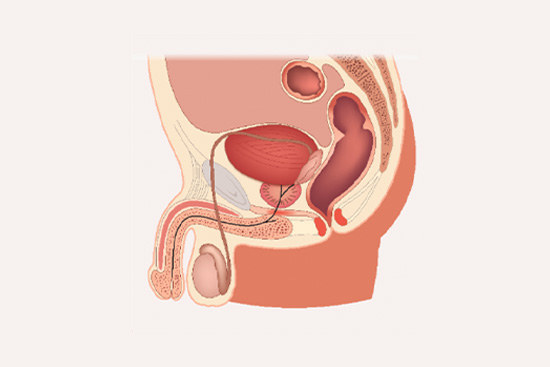
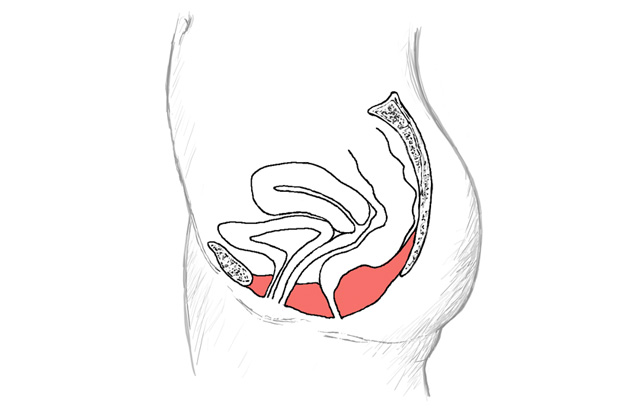
What Every Women Should Know About Her BladderWhere are the Pelvic Floor Muscles?
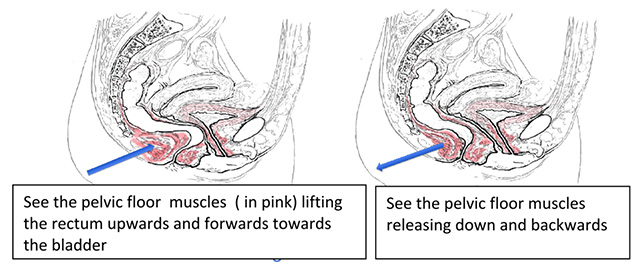
The pelvic floor muscles support the pelvic organs i.e. the bladder, uterus and rectum. These muscles should react automatically to close the bladder outlet when you cough or sneeze. During childbirth, muscles can be damaged and become ineffective resulting in loss of control at the bladder outlet. It is important to know that this can happen even if a woman hasn't given birth vaginally. In the diagram below, the pelvic floor muscles are in pink and can be shown to support the rectum, the uterus and the bladder.
The Pelvic Floor Exercise (Pelvic Floor Elevator)
Every one is different and needs an exercise programme to suit their individual needs. However, this is a good way to activate your muscles as you imagine your pelvic floor is like a lift and try to take the lift up and down to different floors.
- Sit comfortably on an upright chair, knees slightly apart.
- Breathe in deeply and then all the way out.
- Take the lift to the first floor by gently lifting your back passage up and forwards towards your bladder (be careful not to brace your tummy)
- As soon as you have tightened - resume normal breathing while you hold.
- Keep holding for 5 secs and build up to 10 secs.
- Release the muscle completely.
- Breathe in deeply and then all the way out.
- Take the lift to the second floor by contracting your back passage and water passage , as above.
- As soon as you have tightened - resume normal breathing while you hold.
- Next time contract the muscles and take the lift to the third floor.
- Repeat to each floor holding each repetition up to 10 seconds.
- Correct breathing and the ability to release the muscle COMPLETELY to the basement during the programme is very important.
In order to control the bladder and stop accidents you must increase the strength and endurance of the muscles.
- Aim to squeeze harder to take the lift higher.
- Aim to squeeze longer to hold the lift longer at each floor.
- Count how long you can hold for and how many times you can repeat the squeezes. This will enable you to know that you are increasing your exercise programme and improving your strength.
- Aim to hold for 10 seconds and do 10 repetitions as a guide.
- Include a set of fast squeezes in each set of exercises; tighten quickly and release quickly and repeat 10 times - this is to target your fast muscle fibres that will stop you from leaking when you cough)
- Do 10 of your 10 second holds and 10 of your fast contractions three times per day.
- Record your programme to see your progress. The Squeezy Ap is a good way to do this.
Once you have mastered these exercises use them when you need them. Practice holding the muscle and coughing to prevent a leak. This is called 'The Knack'.
Hold While You Cough 'The Knack'
Try to pull up your pelvic floor BEFORE you cough so that it is protected and giving support from below. This is called 'The Knack'. The knack is the most important technique for you to use if you are coughing.
Activities, such as coughing or sneezing increase the intraabdominal pressure, and therefore the downwards pressure on the pelvic floor. Ongoing episodes of coughing may lead to an exacerbation of leakage of urine (stress incontinence), a feeling of heaviness in the vaginal passage (related to prolapse) or lack of control of wind from the back passage. This will be particularly challenging for an already weakened pelvic floor. Many factors contribute to this weakened pelvic floor including child birth, menopausal changes, ongoing heavy lifting and chronic straining to pass a bowel movement.
The first challenge is to connect with your pelvic floor muscles and see if you can feel them working.
- Sit in an upright position with your rib cage over your pelvis and the weight equally distributed through both sit bones.
- Breathe normally. Focus on the muscles connecting from your back passage upwards and forwards to your bladder.
- Just before you cough pull up your pelvic floor muscles. It is the timing of this contraction that is important.
This will help to support the neck of the bladder so that you do not leak, the pelvic organs do not descend and you do not pass wind. All of these take practice but once mastered, should become an automatic reaction to help protect your pelvic floor with coughing or sneezing. If you feel that you cannot control the downwards force, try to support your perineal area with counter pressure from your hand or a small towel roll as you cough.
Repeated coughing can be very tiring, not very effective in clearing your chest and can put downwards strain on the pelvic floor. If you have a chronic respiratory condition or have recently developed a cough please use the techniques above every time.
The Abdominal Muscles (Transversus Abdominis )
The deep muscles of your abdomen support your spine and pelvic floor. These supporting muscles provide a "girdle of strength" around your pelvis and work for long periods of time.
They work most effectively when the pelvis is held in the natural 'neutral' position. To be more effective in doing your exercises aim to find this neutral position. Imagine a compass on your lower abdomen, the navel is north and pubic bone is south. Your pelvic bones are east and west. In neutral, the line between the pubic and pelvic bones remains horizontal. Start your exercise with your pelvis in this position whether you are lying, sitting or standing.
- The abdominal muscles are easiest to find in side lying with the tummy relaxed. Check your pelvis is in neutral whether in lying, sitting or standing.
- Slowly and gently draw in the lower abdominal muscles as if bringing your tummy button towards your spine or think of bringing your hip bones together or pulling your lower tummy away from the zip of your trousers. Don't brace or force your tummy and don't move the spine or pelvis.
- Keep breathing and hold the muscle for at least 10 seconds. Using this abdominal muscle can help you find your pelvic floor muscle. It is not easy to find the pelvic floor muscles and it can take a lot of time and concentration.
NB Bracing the tummy is incorrect; this technique is gentle and slow and the tummy should not bulge out. This slow contraction of the deep abdominal muscle will help a pelvic floor contraction but bracing and forcing will not. It is important to know that over-holding of the abdominal muscles can be part of the problem with bladder overactivity. It is important to release the abdominal muscles as well to ensure correct activation.
Posture
When your posture is correct you will look and feel better. It also enables you to improve the control over the pelvic floor for longer periods of time e.g. when out for a walk.

- Hold your head up but not your chin.
- Lift your breast bone and keep your neck long.
- Breathe down low.
- Keep your pelvis in the neutral position.
- Keep your knees straight, not locked.
- Keep your weight back a little towards your heels.
Bladder Retraining for Urgency or Urge Incontinence
For people who have problems making it to the toilet in time, simple bladder retraining can improve your symptoms. Urge incontinence is due to over-activity of the bladder muscle or nerves. It gives a sensation of urgency to pass urine and you may not reach the toilet in time. Having to get up more than once a night is common.

An average person can hold 400 to 500mls of fluid and passes urine five to eight times in a 24 hour period. When you have a problem with urgency it is usually due to a disturbance in the reflexes of the bladder or reduced bladder size. The bladder gives off strong messages that it wants to empty and you find it difficult to stop the reflex, the bladder squeezes and the pelvic floor is not strong enough to resist it.
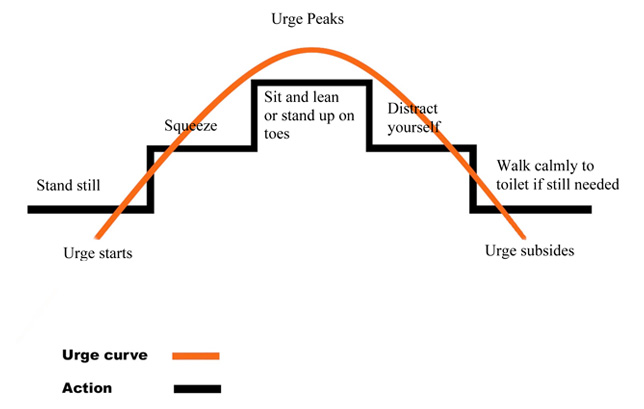
To retrain your bladder, when you feel the urge to go to the toilet during the day try and hold on for a few minutes longer than you normally would before passing urine. Try not to rush to the toilet at the point when your urge is strongest (see diagram). Use the techniques below to practice holding. It can be very difficult at first and seem impossible.
What To Do:
- Stand still or sit down. Sitting and leaning forward is best.
- Press on your pelvic floor muscles underneath and hold the pressure for as long as it takes for the urge to subside.
- If you can't sit - stand up on your toes for a long as it takes for the contraction to subside (this helps settle the reflexes).
- Breathe in a regular pattern.
- Don't brace your stomach.
- Tighten your pelvic floor muscles gently.
- Think of something else other than the toilet - distract yourself, Give yourself a small task to do e.g. check your text messages.
- When the urge subsides you can then walk calmly to the toilet.
Urge Curve
Points To Remember
- Don't go to the toilet "just in case". Learn to take control of your bladder and have confidence.
- Use your muscles when you need them and exercise them regularly.
- The more control you need, the harder you must squeeze - but don't brace!
- Drink 1.5 litres of water a day.
- Avoid large quantities of alcohol, avoid tea and coffee, fizzy drinks and alcohol.
- Watch your weight; being overweight can put a further strain on your muscles.
- Avoid constipation and straining by taking extra fibre in your diet.
- It may take up to 3-5 months to train the muscles and as much as a year.
- Improvements can happen much sooner ie as soon as you change your habits.
- You can always insert two fingers into the vagina to see if you are doing the exercise correctly and for the male press your fingers on the perineum behind the scrotum.
- Keep up your exercises for life - use it or lose it!
Medication
If the urge is too severe then talk to your doctor about medication. You should practice these techniques in conjunction with the drug therapy. Bladder retraining may also be used for someone who has an over stretched bladder.
Bladder Diary
Your doctor, physiotherapist or nurse continence advisor may ask you to fill out a bladder record chart or bladder diary. This is a record of your fluid intake, the amount of fluid passed and episodes of leakage daily. This gives a lot of information about the minimum and the maximum amount of fluid the bladder can hold, types of fluids you are drinking, whether they are irritating the bladder, the number of times you are going to the toilet daily and the different patterns that you have established. This chart will be used to help you and your advisor understand and retrain your bladder.
There is more information available on www.oab.ie and you can download bladder diaries from this website.